ICSI (intracytoplasmic sperm injection)
 ICSI refers to a process whereby a single sperm is injected into an oocyte to facilitate fertilization. ICSI is used when there is a likelihood the sperm may show difficulty in penetrating and fertilizing the oocyte. ICSI may be used to overcome defects in sperm quality such as low sperm numbers, poor forward motility and poor sperm morphology.
ICSI refers to a process whereby a single sperm is injected into an oocyte to facilitate fertilization. ICSI is used when there is a likelihood the sperm may show difficulty in penetrating and fertilizing the oocyte. ICSI may be used to overcome defects in sperm quality such as low sperm numbers, poor forward motility and poor sperm morphology.
Presently the use of ICSI has expanded to cases of repeated IUI failures, male and female patients of older age and sperm with high DNA fragmentation.
ICSI may be used in conjunction with surgical sperm retrieval in cases of obstructed azoospermia. The sperms may be extracted from the husband¡¦s epididymis or testes and fertilization of the woman¡¦s oocytes accomplished using ICSI, producing viable embryos for replacement.
Advanced sperm selection techniques for ICSI
The sperm contributes to half of the genetic material in an embryo and is associated with high implantation rates. Improved sperm selection techniques followed by ICSI are thought to improve the chance that structurally intact and mature sperm with high DNA integrity are selected for fertilization.
Advanced sperm selection techniques include ability to bind to hyaluronic acid; and sperm morphology under ultra-high magnification.
The ability of sperm to bind to hyaluronic acid indicates maturity and high DNA integrity. Hyaluronic acid is a protein found on the outer layer of the oocyte or egg. Hyaluronic acid acts as chemo-attractant that activates and binds mature sperms with intact DNA. Sperms that show binding to hyaluronic acid is selected for ICSI. The technique which select for sperm with normal physiological reaction is known as PICSI i.e. ¡§Physiological ICSI¡¨
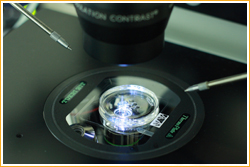
IMSI (intra-cytoplasmic morphological selected sperm injection) uses high magnification of over 6000x times to assess a sperm appearance for abnormalities. The sperm that best fit the morphological criteria is selected for ICSI.
|
Stages of an IVF-ICSI cycle
|
|
Medical Assessment
|
The couple undergoes medical examination, ultrasound assessment, blood tests, semen analysis and other tests as necessary
|
|
Counseling and treatment consent
|
The couple suitable for IVF-ICSI undergoes counseling and signs an informed consent before embarking on treatment
|
|
Controlled ovarian hyperstimulation (COH)
|
COH usually begin on the 2nd or 3rd day of menses. The woman¡¦s pituitary axis is shut down or suppressed using GnRH analogue or GnRH antagonist. Gonadotrophin is given to stimulate the ovaries to produce several follicles containing oocytes.
|
|
Monitoring ovarian response
|
The growth of follicles is monitored via ultrasound tracking. The dosage of gonadotrophin may be adjusted to achieve a satisfactory ovarian response. When the follicles reach a suitable size, an injection of hCG is given to induce oocyte maturity and ovulation.
|
|
Oocyte Pickup (OPU)
|
OPU is usually performed 34-36 hours after hCG injection. The oocytes are aspirated from the follicles under sedation using ultrasound guidance. The procedure usually lasts between 30 -60 minutes. The woman is required to fast 6-8 hours before OPU.
|
|
Semen collection
|
Fresh semen sample is collected from the husband on the day of OPU. The semen sample shall be analyzed and processed to select motile sperms for use in IVF-ICSI. If the husband has difficulty with semen collection, a sample should be frozen and stored before starting treatment.
|
|
IVF-ICSI
|
The couple¡¦s oocytes and sperms are used to produce viable embryos. The use of IVF or ICSI for fertilization shall depend on the quality of available sperms. Advance sperm selection technique used with ICSI is advised if the sperm quality is poor.
|
|
Embryo culture
|
The fertilized oocytes are cultured until they become embryos. The development of embryos is assessed regularly to facilitate selection of good quality embryos.
|
|
Embryo transfer (ET)
|
One to three embryos may be replaced into uterus depending on prognosis and age of the woman. If the woman¡¦s condition is unsuitable for ET, the embryos may be frozen and stored for future replacement.
|
|
Luteal support
|
Progesterone pessaries, progesterone injections and/or hCG injections may be used to improve uterine lining and assist embryonic implantation.
|
|
Early pregnancy test
|
The earliest positive indication of pregnancy is by blood test for the beta hCG 12-14 days after ET.
|